HOW RED COMPLEX BACTERIA ACT IN PATIENTS WITH RHEUMATOID ARTHRITIS, WHO HAVE DENTAL IMPLANTS
DOI:
https://doi.org/10.61164/rmnm.v4i1.3605Keywords:
BACTÉRIAS DO COMPLEXO VERMELHOAbstract
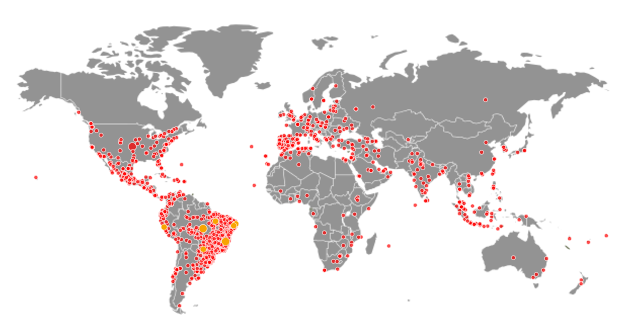
Introduction: The search for an aesthetic and functional smile has been increasingly promoted by treatments with dental implants, providing effectiveness for edentulous patients. However, for a good prognosis, a good oral bone structure is necessary, which can be impaired by bacteria present in the pathology that affects the periodontium, periodontitis. Furthermore, rheumatoid arthritis also becomes an etiological factor for poor bone adherence, due to its autoimmune inflammatory process. Objective: To elucidate the interaction of the red bacterial complex, periodontitis, and the repercussions of rheumatoid arthritis in implantology, aiming to promote the study of osseointegration in dental implants. Methodology: This is an integrative literature review, qualitative in nature, with a descriptive approach, conducted in January 2025. Data collection was done by surveying articles on the SCIELO (Scientific Electronic Library Online), PUBMED (National Center for Biotechnology Information NCBI), and BVS (Virtual Health Library) platforms. The descriptors used were: Rheumatoid arthritis, dental implants, bacterial complex, and periodontitis. As inclusion criteria, studies published between 2005 and 2024 in Portuguese and English were used. Duplicated studies in the aforementioned databases were excluded, as well as conference abstracts and letters to the editor. Results: Scientifically, the importance of a healthy structure at the level of the alveolar ridge and facial bones is attested for implantology to succeed in its reparative function. In this aspect, the structure of the insertion periodontium must be preserved; however, periodontitis causes inflammation in the region, and the red bacterial complex of this pathology can accelerate its progression because bacterial membrane vesicles promote bone resorption. This, along with the distance from the amelocementary junction and the spacing of the alveolar bone crest, is caused by an increase in cellular apoptosis in contact with the bacterial complex. Moreover, rheumatoid arthritis influences bone cell resorption and remodeling, negatively affecting the clinical prognosis for dental implants, as there is an excessive production of osteoclasts, which promote bone resorption. In scientific aspects, studies do not reach exact consensus on the interference of the bacterial complex itself, but rather its influence on periodontitis, which can be associated with the symptoms of rheumatoid arthritis. Conclusion: The effectiveness of dental implants is based on a good oral environment, with preserved bone aspects. Regarding the activity of bacteria from the bacterial complex, rheumatoid arthritis, and periodontitis as factors altering the efficiency of implantology, further scientific investigation is needed to clarify how these organisms interact in the human system, as the implant market continues to grow and people, driven by the desire to restore their smiles, seek the success of these procedures.
References
Holt, S. C.; Ebersole, J. L. Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia: the "red complex", a prototype polybacterial pathogenic consortium in periodontitis. Periodontology 2000, 38, 72–122. 2005. https://doi.org/10.1111/j.1600-0757.2005.00113.x
Silva et al. Correlação entre a expressão de Osteocalcina e a de marcadores da reabsorção óssea (Rank, RankL E OPG) em sítios implantáveis das maxila e mandíbula. Faculdade de Odontologia - UFG, 2011.https://www.sbpcnet.org.br/livro/63ra/conpeex/pivic/trabalhos/DONIZETE.PDF
Scott, David L et al. “Rheumatoid arthritis.” Lancet (London, England) vol. 376,9746 (2010).https://pubmed.ncbi.nlm.nih.gov/20870100/
Kim, J.-E. Osteoclastogenesis and osteogenesis. International journal of molecular sciences, v. 23, n. 12, p. 6659, 2022.https://pubmed.ncbi.nlm.nih.gov/35743101/
Guglielmotti, M. B, et al. Research on implants and osseointegration. Periodontology 2000, v. 79, n. 1, p. 178–189, 2019.https://pubmed.ncbi.nlm.nih.gov/30892769/
Hao, C.-P. et al. The osseointegration and stability of dental implants with different surface treatments in animal models: a network meta-analysis. Scientific reports, v. 11, n. 1, 2021.https://pubmed.ncbi.nlm.nih.gov/34226607/
Monje, A. et al. Alveolar bone architecture: A systematic review and meta‐analysis. Journal of periodontology, v. 86, n. 11, p. 1231–1248, 2015. https://pubmed.ncbi.nlm.nih.gov/26177631/
Gaudy, Jean-François. Atlas de Anatomia para Implantodontia. Grupo GEN, 2014. E-book. ISBN 9788595152830. https://www.grupogen.com.br/e-book-atlas-de-anatomia-para-implantodontia-jean-francois-gaudy-bernard-cannas-luc-gillot-thierry-gorce-e-jean-luc-charrier-9788535269857?srsltid=AfmBOoru1n9klNdRNImgZW6tOrdwARSxA12vo57DwVHW9JsQ-fF9LBZQ
Ajanovic´, M. et al. Radiographic evaluation of crestal bone loss around dental implants in maxilla and mandible: One-year prospective clinical study. Acta stomatologica Croatica, v. 49, n. 2, p. 128–136, 2015. https://pubmed.ncbi.nlm.nih.gov/27688395/
Mikuls, T. R. et al. Periodontitis andPorphyromonas gingivalisin Patients With Rheumatoid Arthritis. Arthritis & Rheumatology, v. 66, n. 5, p. 1090–1100, 28 abr. 2014. https://pubmed.ncbi.nlm.nih.gov/24782175/
Berglundh, T. et al. Etiology, pathogenesis and treatment of peri-implantitis: A European perspective. Periodontology 2000, 2 fev. 2024. https://pubmed.ncbi.nlm.nih.gov/38305506/
AMADOR SALOMÃO, P. E. .; TEIXEIRA OLIVEIRA SANTOS, A. . EVOLUÇÃO E DESAFIOS NA AVALIAÇÃO CIENTÍFICA: DA CLASSIFICAÇÃO DE PERIÓDICOS À QUALIDADE INTRÍNSECA DOS ARTIGOS. Revista Multidisciplinar do Nordeste Mineiro, [S. l.], v. 1, n. 1, p. 1–18, 2025. DOI: 10.61164/rmnm.v1i1.3481
Fan, R. et al. Porphyromonas gingivalis Outer Membrane Vesicles Promote Apoptosis via msRNA-Regulated DNA Methylation in Periodontitis. Microbiology Spectrum, v. 11, n. 1, 14 fev. 2023.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista Multidisciplinar do Nordeste Mineiro

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.