SEROMA IN THE CONTEXT OF BREAST CANCER AND THE INSERTION OF THE NURSE: INTEGRATIVE LITERATURE REVIEW
DOI:
https://doi.org/10.61164/rmnm.v1i3.3551Keywords:
Seroma, Breast neoplasms, Nursing care, Perioperative nursing, Oncology nursingAbstract
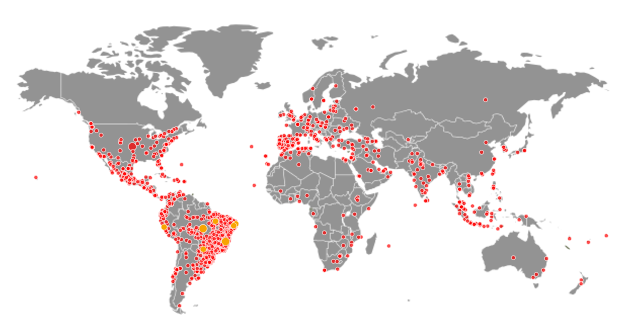
Seroma is one of the most frequent postoperative complications in the nursing care context for patients undergoing breast cancer treatment. This study aimed to identify, in the scientific literature, evidence regarding the involvement of nurses in caring for women with seroma treated for breast cancer. An integrative review was conducted by searching the PubMed, Cinahl, Scopus, Embase, and LILACS databases. Ten articles were selected according to the eligibility criteria, and the review was reported following the PRISMA guidelines. Most of the studies (70.0%) were published in Europe, 20.0% in South America, and 10.0% in North America, with a notable prevalence of prospective observational studies. The nurse’s role was synthesized into two categories: Postoperative follow-up: Nurses play a crucial role in monitoring and the early detection of complications, such as seroma accumulation, as well as in providing psychosocial support. This follow-up can take place in outpatient settings, through teleconsultations, home visits, or telephone contact, with nurses offering guidance on drain management, pain control, arm exercises, and the use of prostheses. Interventions for seroma management: Nursing actions include dressing changes and, most importantly, percutaneous aspiration after identifying fluctuant areas. The establishment of nurse-led services for seroma aspiration has been reported in several countries, along with the creation of protocols and training programs. In summary, the integration of nurses into the care of breast cancer patients with seroma involves both postoperative follow-up—aimed at early detection of complications—and direct interventions for seroma control, such as dressing procedures and percutaneous aspiration.
References
American Cancer Society. Breast Cancer Facts & Figures 2022-2024 [Internet]. 2022 [citado em 22 de março de 2023];18:1-9. Disponível em: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/2022-2024-breast-cancer-fact-figures-acs.pdf.
Boman L, Lindgren A, Sandelin K. Women's perceptions of seroma and their drainage following mastectomy and axillary lymph node dissection. Eur J Oncol Nurs [Internet]. 2002 [citado em 22 de março de 2023];6(4):213-9. Disponível em: https://pubmed.ncbi.nlm.nih.gov/12849580/. DOI: 10.1054/ejon.2002.0186.
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin [Internet]. 2018 [citado em 22 de março de 2023];68(6):394-424. Disponível em: https://bmccancer.biomedcentral.com/articles/10.1186/s12885-020-07242-0. DOI: 10.3322/caac.21492.
Charlton J. Developing a nurse-led service. Journal of Community Nursing. [Internet]. 2002 [citado em 22 de março de 2023]:13-16. Disponível em: https://www.jcn.co.uk/resources/all/0/date/desc/topic/Training
Conselho Regional de Enfermagem de Santa Catarina. Parecer CorenSC Nº 003CT2013. Solicitação de Parecer Técnico acerca da aspiração de seroma em pacientes mastectomizadas por profissional de enfermagem. [Internet]. 2013 [citado em 22 de março de 2023]. Disponível em: https://www.corensc.gov.br/wp-content/uploads/2015/07/Parecer-003-2013-CT.pdf.
Cruz LAP, Prado MAS, Ferreira SM. Ocorrência de seroma pós-mastectomia e o cuidado com o dreno aspirativo no domicílio. Rev enferm UFPE on line [Internet]. 2017 [citado em 22 de março de 2023];11(1):179-87. Disponível em: https://periodicos.ufpe.br/revistas/revistaenfermagem/article/view/11892. DOI: https://doi.org/10.5205/1981-8963-v11i1a11892p179-187-2017.
dos Santos Scofano B, Almeida de Lima A, dos Reis Silva R, et al. Ações/plano de alta da enfermagem à mulher submetida à mastectomia. Nursing (São Paulo) [Internet]. 2020 [citado 6 de abril de 2023];23(263):3736-44. Disponível em: https://www.revistanursing.com.br/index.php/revistanursing/article/view/670. DOI: https://doi.org/10.36489/nursing.2020v23i263p3736-3744.
Eliav T, Novack V, Krieger Y. Effect of quilting on seroma formation in mastectomies: A meta-analysis. Surg Oncol [Internet]. 2021 [citado em 06 de abril de 2023];39:101665. Disponível em: https://linkinghub.elsevier.com/retrieve/pii/S0960-7404(21)00154-7. DOI: 10.1016/j.suronc.2021.101665.
Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today [Internet]. France: International Agency for Research on Cancer; 2020 [citado em 22 de março de 2023]. Disponível em: https://gco.iarc.fr/today.
Huang J, Wang S, Wu Y, et al. Conventional suture with prolonged timing of drainage is as good as quilting suture in preventing seroma formation at pectoral area after mastectomy. World J Surg Oncol [Internet]. 2021 [citado em 22 de março de 2023];19(1):148. Disponível em: https://pubmed.ncbi.nlm.nih.gov/33980267/. DOI: 10.1186/s12957-021-02257-8.
Huttunen T, Leidenius M, Jahkola T, et al. Delay in the initiation of adjuvant chemotherapy in patients with breast cancer with mastectomy with or without immediate breast reconstruction. BJS open. [Internet]. 2022 [citado em 03 de março de 2023]; 6(4):1-6. Disponível em https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9366640/pdf/zrac096.pdf. DOI: https://doi.org/10.1093/bjsopen/zrac096.
Instituto Nacional de Câncer. Estimativa 2023: incidência de câncer no Brasil. Rio de Janeiro: INCA, 2022. [citado em 22 de março de 2023]. Disponível em: https://www.inca.gov.br/publicacoes/livros/estimativa-2023-incidencia-de-cancer-no-brasil.
Koivisto JM, Saarinen I, Kaipia A, et al. Patient education in relation to informational needs and postoperative complications in surgical patients. Int J Qual Health Care. [Internet]. 2019 [citado em 22 de março de 2023];32(1):35-40. Disponível em: https://pubmed.ncbi.nlm.nih.gov/31016323/. DOI: 10.1093/intqhc/mzz032.
Marchal F, Dravet F, Classe JM, et al. Post-operative care and patient satisfaction after ambulatory surgery for breast cancer patients. Eur J Surg Oncol [Internet]. 2005 [citado em 22 de março de 2023];31(5):495-9. Disponível em: https://pubmed.ncbi.nlm.nih.gov/15922885/. DOI: 10.1016/j.ejso.2005.01.014.
McLaughlin SA, Brunelle CL, Taghian A. Breast cancer-related lymphedema: risk factors, screening, management, and the impact of locoregional treatment. J Clin Oncol. [Internet]. 2020 [citado em 22 de março de 2023];38(20):2341-50. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32442064/. DOI: 10.1200/JCO.19.02896.
Mertz BG, Kroman N, Williams H, et al. Fast-track surgery for breast cancer is possible. Dan Med J [Internet]. 2013 [citado em 22 de março de 2023];60(5):A4615. Disponível em: https://pubmed.ncbi.nlm.nih.gov/23673259/.
Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2022. CA Cancer J Clin [Internet]. 2022 [citado em 22 de março de 2023]; 72(5):409-36. Disponível em: https://pubmed.ncbi.nlm.nih.gov/35736631/. DOI: 10.3322/caac.21731.
Montagna G, Zhang J, Sevilimedu V, et al. Risk Factors and Racial and Ethnic Disparities in Patients With Breast Cancer-Related Lymphedema. JAMA Oncol. [Internet]. 2022 [citado em 22 de março de 2023]; 8(8):1195-1200. Disponível em: https://pubmed.ncbi.nlm.nih.gov/35679026/. DOI: 10.1001/jamaoncol.2022.1628.
Mourregot A, Leclerc G, Ducreux L, et al. Ambulatory mastectomy for cancer: feasible and safe in consenting educated patients in a care network. Ethics Med Public Health [Internet]. 2021 [citado em 22 de março de 2023];18:1-9. Disponível em: https://www.sciencedirect.com/science/article/abs/pii/S2352552521000499. DOI: https://doi.org/10.1016/j.jemep.2021.100672.
Nzenwa IC, Iqbal HA, Hardie C, et al. Wound complications following surgery to the lymph nodes: A protocol for a systematic review and meta-analysis. PLoS ONE [Internet]. 2022 [citado em 06 de abril de 2023];17(8):e0272490. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9348652/. DOI: https://doi.org/10.1371/journal.pone.0272490.
O'Hea BJ, Ho MN, Petrek JA. External compression dressing versus standard dressing after axillary lymphadenectomy. Am J Surg [Internet]. 1999 [citado em 22 de março de 2023];177(6):450-3. Disponível em: https://pubmed.ncbi.nlm.nih.gov/10414691/. DOI: 10.1016/s0002-9610(99)00089-6.
Petito EL, Esteves MT, Elias S, et al. The influence of the initiation of an exercise programme on seroma formation and dehiscence following breast cancer surgery. J Clin Nurs [Internet]. 2014 [citado em 22 de março de 2023];23(21-22):3087-94. Disponível em: https://pubmed.ncbi.nlm.nih.gov/24479839/. DOI: 10.1111/jocn.12544.
Pinto C da S, Borsatto AZ, Vaz DC, et al. Telemedicina em Cuidados Paliativos Oncológicos: um Legado da Pandemia. Rev. Bras. Cancerol. [Internet]. 31 de janeiro de 2023 [citado 4 de abril de 2023];69(1):e-142698. Disponível em: https://rbc.inca.gov.br/index.php/revista/article/view/2698. DOI: https://doi.org/10.32635/2176-9745.RBC.2023v69n1.2698.
AMADOR SALOMÃO, P. E. .; TEIXEIRA OLIVEIRA SANTOS, A. . EVOLUÇÃO E DESAFIOS NA AVALIAÇÃO CIENTÍFICA: DA CLASSIFICAÇÃO DE PERIÓDICOS À QUALIDADE INTRÍNSECA DOS ARTIGOS. Revista Multidisciplinar do Nordeste Mineiro, [S. l.], v. 1, n. 1, p. 1–18, 2025. DOI: 10.61164/rmnm.v1i1.3481.
Ribeiro LC, Boechat VT, Aguiar SFC, et al. O desenvolvimento do linfoma anaplásico de células grandes associado ao implante mamário em mulheres. Brazilian Journal of Surgery and Clinical Research [Internet]. 2021 [citado em 22 de março de 2023];36(1):53-62. Disponível em: https://www.mastereditora.com.br/periodico/20210906_133639.pdf.
Rooij L, Kuijk SMJV, Haaren ERMV, et al. A single center, randomized, non inferiority study evaluating seroma formation after mastectomy combined with flap fixation with or without suction drainage: protocol for the seroma reduction and drain free mastectomy (SARA) trial. BMC Cancer [Internet]. 2020 [citado em 22 de março de 2023];20(1):735. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32767988/. DOI: 10.1186/s12885-020-07242-0.
Scomacao I, Cummins A, Roan E, et al. The use of surgical site drains in breast reconstruction: A systematic review. J Plast Reconstr Aesthet Surg [Internet]. 2022 [citado em 06 de abril de 2023];73(4):651-662. Disponível em: https://pubmed.ncbi.nlm.nih.gov/31926896/. DOI: 10.1016/j.bjps.2019.11.019.
Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and metaanalysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. DOI: https://doi.org/10.1136/bmj.g7647.
Souza MT, Silva MD, Carvalho R. Integrative review: What is it? How to do it? Einstein (São Paulo). 2010;8(1):102-6. DOI: https://doi.org/10.1590/S1679-45082010RW1134.
Turner EJ, Benson JR, Winters ZE. Techniques in the prevention and management of seromas after breast surgery. Future Oncol [Internet]. 2014 [citado em 22 de março de 2023];10(6):1049-63. Disponível em: https://pubmed.ncbi.nlm.nih.gov/24941989/. DOI: 10.2217/fon.13.257.
Unger J, Rutkowski R, Kohlmann T, et al. Potential risk factors influencing the formation of postoperative seroma after breast surgery - A prospective study. Anticancer Res [Internet]. 2021 [citado em 22 de março de 2023];41(2):859-67. Disponível em: https://pubmed.ncbi.nlm.nih.gov/33517291/. DOI: 10.21873/anticanres.14838.
Vos H, Smeets A, Neven P, et al. Early drain removal improves quality of life and clinical outcomes in patients with breast cancer - Results from a randomised controlled trial. Eur J Oncol Nurs [Internet]. 2018 [citado em 22 de março de 2023];36:112-18. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30322501/. DOI: 10.1016/j.ejon.2018.08.007.
Warren M. Collaboration in developing a protocol for nurse-led seroma aspiration. Br J Nurs. [Internet]. 2008 [citado em 22 de março de 2023];17(15):956-60. Disponível em: https://pubmed.ncbi.nlm.nih.gov/18983016/. DOI: 10.12968/bjon.2008.17.15.30697.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista Multidisciplinar do Nordeste Mineiro

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.